What is a total knee replacement?
Total knee replacement is a common procedure to replace a diseased or severely injured knee joint.
Common reasons for replacing a knee joint include:
Severe osteoarthritis – Degeneration of joint cartilage and the underlying bone, causing pain and stiffness
Ligament damage – Damage to the ligament or infection that leads to severe osteoarthritis
Rheumatoid arthritis – A chronic progressive disease causing inflammation in the joints
Crystal deposition diseases – Diseases such as gout and ‘pseudogout’ that can cause arthritis
Avascular necrosis – Death of bone following loss of blood supply
Bone dysplasias – Disorders of the growth of bone.
Source – Better Health
Knee replacement
When your knee joint is damaged it may develop arthritis.
Arthritis causes the cartilage surfaces of the knee joint, which are usually very smooth to become rough and deformed. This means the surface of the end of the thighbone and top of the shin bone no longer match each other causing the movement of the knee to be abnormal and for the knee to become bow legged or knock-kneed.
In some parts of the knee joint all the cartilage may be worn away and bone rubs on bone. This causes increasing pain, deformity and stiffness.
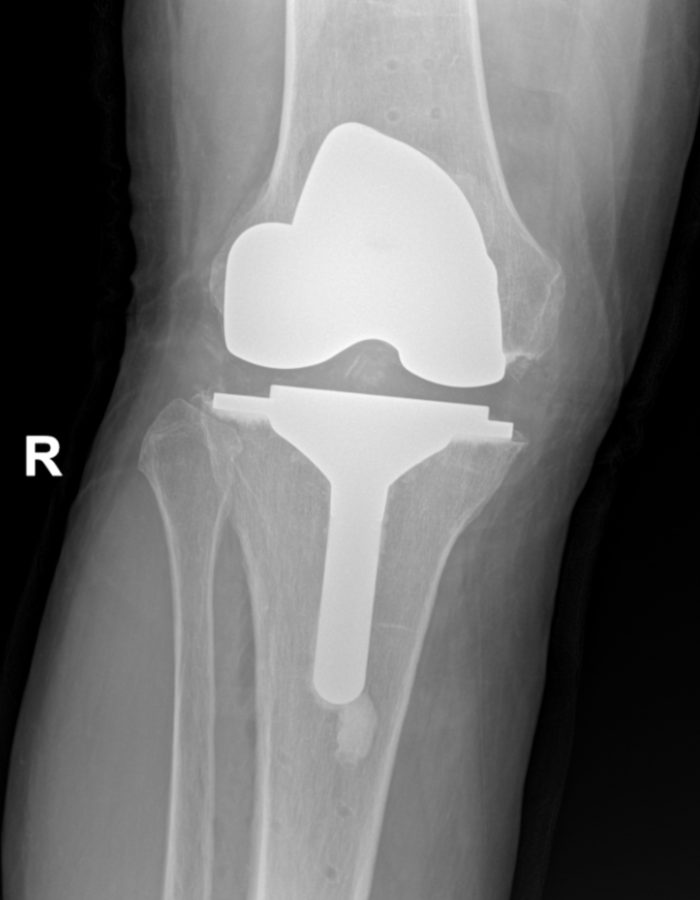
A total knee replacement is when the old diseased knee joint is replaced with a new metallic knee joint.
During a total knee replacement:
- The end of your thighbone is shaved off and replaced with a metal shell.
- The top of the lower shin is also removed and replaced with a metal shell.
- The space between the two metal caps is then filled with a plastic surface.
- The surface of the kneecap is always replaced as well.
This provides a smoother, pain free and more mobile joint. These parts are cemented into place and you can begin using them straight away after the surgery.
Knee replacement operation
How long does it take?
The knee replacement operation takes around one and a half hours. You are taken to theatre about one hour before the procedure starts. Here the anaesthetist will put you to sleep and numb your leg for surgery. After the operation you will remain in the recovery area for around one hour.
Anaesthetic
The safest anaesthetic will be worked out between you and the anaesthetist. Usually this will mean an injection into your back with an anaesthetic that numbs your legs. During the operation the anesthetist also puts you into a light sleep. At the end of the operation, you will also have anaesthetic injected into the area of the operation to help keep the area numb from pain.

Incision
The incision is placed over the front of the knee and measures about 15cm-20cm and curves slightly around the kneecap.
The bigger the knee, the longer the incision. Usually there is a patch of numbness about the size of a hand just on the outer part of the incision after the operation. This is because the skin nerves in the area of the incision are cut when the incision is made. This numbness reduces in size afterwards but may not go away completely. It will not affect the function of the knee, and it will become less noticeable with time.
During the operation
A catheter may be placed into the bladder to drain urine. Occasionally, a small plastic drain tube will come from the operated area to take away old blood that collects there after surgery. Compression stockings will be used to help keep the blood flowing from the legs to the heart.
It is important to move your ankles and legs are soon as possible after the anaesthetic as this will help to reduce blood clots in the legs. Straight after the surgery, oxygen will be given for a day or so, antibiotics which help to reduce the risk of infection will be given and blood thinners will be given by injection to reduce blood clots.
Knee Replacement Melbourne – Potential Complications
Joint Infection – Joint infection may occur in less than 1% of cases. To minimise this risk, you will be given antibiotics at the time of surgery and for 48 hours afterwards. This is usually given through a drip. If there are special reasons, you may have an antibiotic continued for a longer period. If an infection occurs despite these precautions, you may need to go back to theatre to have the area washed out. Very occasionally, the knee joint may have to be removed and the operation repeated in the future.
Blood Clots – Blood clots in the legs may occur so this risk is reduced by giving you blood thinners via injection, using compression calf stockings and also a calf or foot massaging devices to increase the flow of blood from your legs to your heart. You can help by being mobile as soon as possible.
Pneumonia – Pneumonia sometimes occurs in patients who spend long periods in bed. When you lie down for long periods of time, your lungs collapse and sputum gets trapped in the squashed part of the lungs. You can prevent this by getting up soon after surgery and being as mobile as possible. If you get pneumonia, you will need antibiotics.
Heart Attack, Kidney Failure and Stroke – Heart attack, kidney failure and stroke may sometimes occur. To minimise the risk, all patients will be assessed before surgery and if there are any particular risk factors, these will need to be looked at before surgery to make you as fit as possible. A physician will look after you for this, and also after to make sure you remain as fit as possible. It is important to let your surgeon and physician know if there are any important aspects to your medical history before your surgery.
Nerve and vessel injury – Injuries to major nerves or vessels may occur but are rare. Should these occur, this may result in weakness of the leg. All standard precautions will be taken to prevent this. Should they occur, a specialist may be called to provide advice and management of that specific complication.
Stiffness and Pain – Stiffness and pain sometimes occurs following a knee replacement. It is important that you use as much painkiller as you need to bring the pain under control and allow you to exercise your knee. You are responsible for your own knee movement and must push yourself to get as much movement as possible.
Post Operative Recovery
Usually you will be up on your feet the day of surgery. This may seem a little early, but it is important to get the body back to normal as soon as possible. We encourage you to be as mobile as possible.
Delays in getting up can sometimes cause problems such as pressure sores on buttocks and heels, pneumonia, blood clots and low blood pressure. Dizziness the first few times of trying to get up from bed is normal. A short rest or movement of your legs will help you to regain your blood pressure. Drinking lots of fluid before you get up will also help.
The physiotherapist and ward staff will help get you up. First you will stand, and if this occurs without problems, then you will walk a few steps with a walking frame. We encourage you to stand and walk using crutches as soon as possible. We hope to have you heading home (or to rehab) approximately 3-4 days after surgery.
Discharge & Rehabilitation
Usually, you will be sent home in your own car. If you feel unsure about heading home (e.g. if you live alone), an assessment will be made to see if you should go to Rehabilitation. This assessment is made by the hospital Physiotherapist and an appropriate rehabilitation centre chosen for you. You will have a post operative appointment scheduled for you 6 weeks after your operation.
Your New Knee
Your new knee should last between 10 to 15 years; avoiding jumping, running and lifting heavy weights may prolong this. Sometimes your activity is sufficient to shake the knee free and so it would have to be revised again. Revision surgery is not as easy as doing it the first time, so please look after your new knee.
KNEE REPLACEMENT – MELBOURNE
Professor Peter Choong specialises in knee replacement surgery and consults with patients from Melbourne and commonly sees patients from interstate and overseas. He has over 30 years of surgical experience and is a Fellow of the Royal Australasian College of Surgeons. Professor Choong is a distinguished surgical leader who has dedicated his career to improving treatments for musculoskeletal diseases.